STIs: Debunking Myths, Fighting Stigma, and Practicing Safer Sex

Sexually transmitted infections (STIs) are more common than most people admit. One in four Australians will get an STI before they turn 25. Yet, many still believe the old myths-that you can tell if someone has an STI just by looking at them, or that only ‘reckless’ people get them. The truth? STIs don’t care about your job, your income, or how many partners you’ve had. They spread because people don’t have accurate information, not because they’re ‘bad’ or ‘dirty.’
It’s easy to get distracted by sensationalized online content. You might scroll past an ad for an escort girl in uk and wonder why it’s even there. But here’s the connection: both topics deal with stigma around sexuality. Whether it’s judging someone for hiring an escort or assuming someone with an STI is promiscuous, the same fear-driven thinking drives both. Real sexual health starts with facts, not shame.
Myths That Still Spread Like an STI
Let’s clear up the biggest lies you’ve probably heard:
- Myth: You’ll know if you have an STI because you’ll feel symptoms. Truth: Chlamydia and gonorrhea often show zero symptoms-especially in women. Up to 70% of women with chlamydia don’t know they have it until it causes damage.
- Myth: Oral sex is safe. Truth: Herpes, gonorrhea, and syphilis can all be passed through oral contact. You don’t need penetrative sex to catch an STI.
- Myth: Condoms are 100% effective. Truth: They reduce risk by 80-95% depending on the STI, but they don’t cover all skin areas. Herpes and HPV can spread from skin not covered by a condom.
- Myth: Only young people get STIs. Truth: Rates among people over 50 have doubled in the last decade. Many divorcees or widows start dating again and don’t think about testing.
These myths aren’t harmless. They keep people from getting tested, delay treatment, and make it harder to talk openly with partners.
Why Stigma Is the Real Epidemic
Stigma kills. Not with viruses, but with silence. When someone gets diagnosed with an STI, their first reaction isn’t usually medical-it’s fear of judgment. They worry about being called ‘dirty,’ ‘slutty,’ or ‘irresponsible.’
That fear stops people from telling partners. It makes them avoid clinics. It leads to untreated infections that can cause infertility, chronic pain, or even increase HIV risk.
And the worst part? The stigma isn’t just from strangers. It’s from doctors who roll their eyes, partners who blame them, and media that paints STIs as punishment. In Australia, a 2024 study found that 62% of people diagnosed with an STI didn’t tell anyone-not even their doctor-until symptoms got worse.
Stigma doesn’t protect public health. It undermines it.
What Safer Sex Actually Looks Like
Safer sex isn’t about perfection. It’s about reducing risk, not eliminating it. Here’s what works:
- Get tested regularly: If you’re sexually active, get checked at least once a year. If you have new or multiple partners, test every 3-6 months. Most clinics offer free or low-cost testing.
- Use condoms and dental dams: Use them every time. Even if you’re on birth control, that doesn’t protect against STIs.
- Talk before you get intimate: Ask your partner when they were last tested. Share your own results. It’s awkward at first, but it builds trust.
- Know your vaccines: HPV and hepatitis B vaccines are highly effective. HPV alone causes 90% of anal and cervical cancers. Get them if you haven’t already.
- Don’t rely on withdrawal or ‘just this once’: Pre-cum can carry chlamydia and gonorrhea. There’s no safe exception.
It’s not about being paranoid. It’s about being responsible. Just like wearing a seatbelt doesn’t mean you expect a crash, using protection doesn’t mean you think your partner is risky-it means you care about both of you.

Testing Is Simple. And Free.
Many people avoid testing because they think it’s complicated, embarrassing, or expensive. It’s not.
In Australia, most public sexual health clinics offer:
- Free urine tests for chlamydia and gonorrhea
- Quick blood tests for HIV, syphilis, and hepatitis
- Self-swab kits for genital herpes and HPV
- Confidential results-no one else sees your records
You don’t need a referral. You don’t need to be a citizen. You don’t even need to give your real name. Most results come back in under a week. And if you test positive? Treatment is often a single pill.
There’s no shame in testing. The only shame is pretending you’re not at risk when you are.
How to Talk to Your Partner
Asking someone about STIs can feel like asking them about their salary. But it doesn’t have to be awkward.
Try this:
- Start with your own status: “I got tested last month and my results were clear. I’d like to know yours before we go further.”
- Make it normal: “A lot of people I know get tested before new partners. It’s just part of being responsible.”
- Don’t accuse: Say “we,” not “you.” “We should both get checked before we stop using condoms.”
- Offer to go together: Many clinics let you book joint appointments.
If someone reacts badly? That says more about them than you. A partner who shames you for wanting to be safe isn’t a partner you should trust.
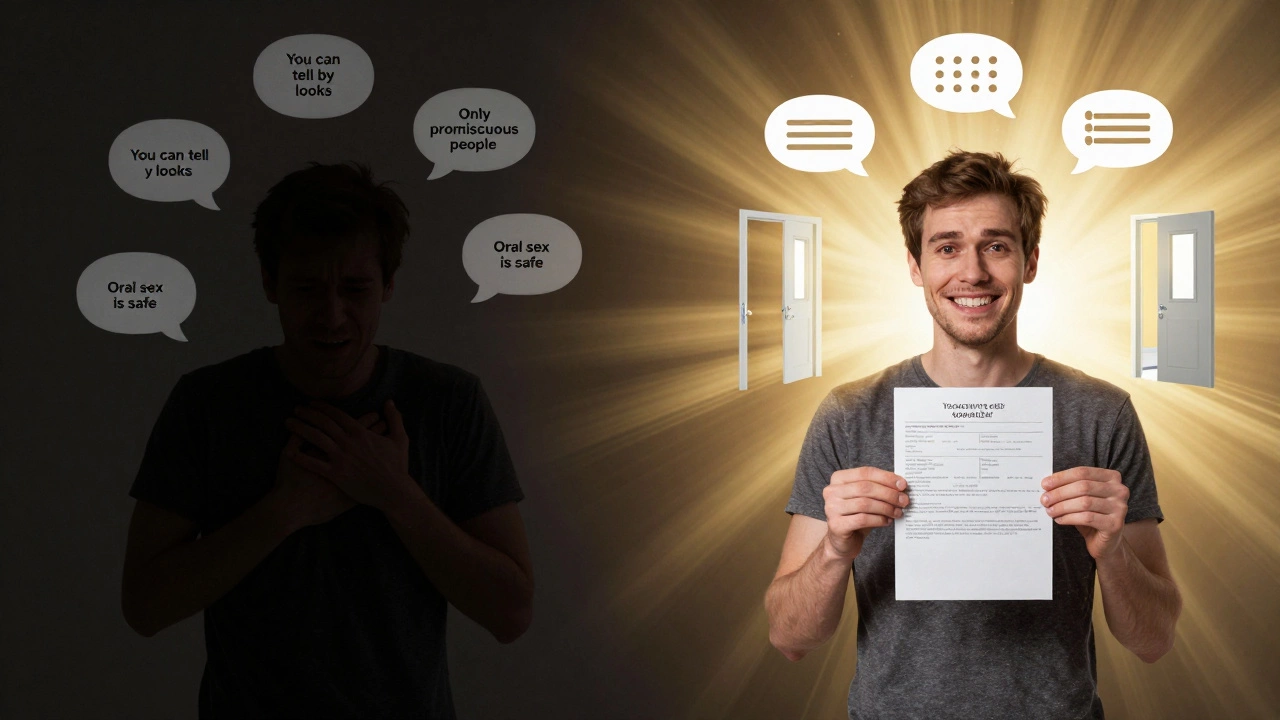
Where Misinformation Comes From
Why do these myths stick? Because they’re repeated everywhere.
TV shows show characters getting diagnosed and then being shunned. Pornography shows unprotected sex as the norm. Social media influencers promote ‘natural’ lifestyles that ignore medical advice. Even some health campaigns use fear-based messaging that backfires.
And then there’s the internet. You’ll find articles claiming ‘natural remedies’ cure herpes or that ‘only promiscuous people’ get HIV. These aren’t just wrong-they’re dangerous. They delay treatment and spread guilt.
Real health information comes from clinics, government health sites, and peer-reviewed science-not TikTok trends or forum posts.
What You Can Do Right Now
You don’t need to wait for a crisis to act. Here’s your quick checklist:
- Book a test if you haven’t had one in the last year
- Keep condoms in your bag, car, or nightstand
- Text a friend: “Hey, when was your last STI test?”
- Share a fact on social media: “You can get chlamydia from oral sex. Here’s what you need to know.”
- Call a clinic and ask what tests they offer-no appointment needed
Small steps add up. One person getting tested can prevent five more infections. One honest conversation can break the cycle of silence.
And if you’re reading this because you’re scared you might have an STI? You’re not alone. You’re not broken. You’re human. And the next step? Get tested. It’s easier than you think.
One more thing: if you’re curious about how sexual health intersects with other parts of life-like dating apps, sex work, or online communities-you’re not alone. The same stigma that surrounds STIs also shows up in places like uk glamour girl escort discussions, where people are judged for choices that have nothing to do with their health. Breaking stigma in one area helps break it everywhere.
Resources You Can Trust
Stick to these sources for accurate info:
- Family Planning Australia (www.familyplanning.org.au)
- Australian Government Department of Health
- Ending HIV (www.endinghiv.org.au)
- QLife (1800 184 527) for LGBTQ+ support
They’re free, confidential, and backed by decades of research-not opinions.
And if you’re still unsure where to start? Walk into a clinic. Say, “I’m here to get tested.” That’s all you need to say.
STIs don’t define you. Silence does.
Get tested. Talk honestly. Protect yourself and others. That’s all safer sex really is.
And yes, if you’re wondering about the connection between STIs and online adult services-yes, it’s real. People in those industries face higher stigma and often lack access to care. That’s why community clinics offer outreach programs. But that’s not an excuse to judge. It’s a reason to support better access for everyone. That’s why the same principles of testing, honesty, and safety apply across the board.
It’s not about who you sleep with. It’s about how you protect each other.